Medical Imaging, Biomarkers Predict PTSD After Brain Injury
Using medical imaging techniques, researchers have found potential brain biomarkers of PTSD in people with traumatic brain injury.
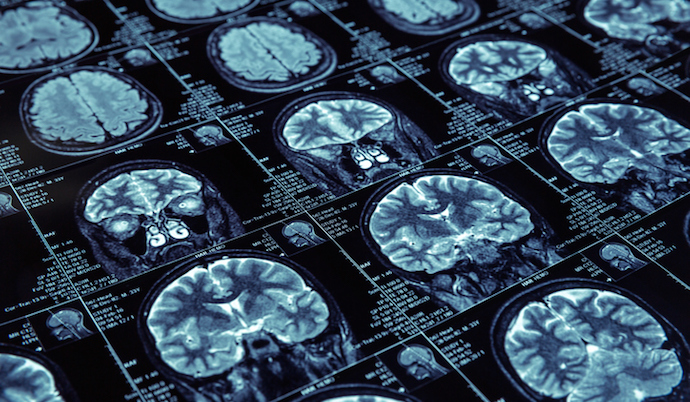
Source: Thinkstock
- Medical imaging techniques helped researchers discover a brain biomarker that may increase a person’s risk of developing post-traumatic stress disorder (PTSD) after a traumatic brain injury, according to a study published in Biological Psychiatry: Cognitive Neuroscience and Neuroimaging.
PTSD is a complex psychiatric disorder brought on by physical and psychological trauma. Symptoms can include depression, anxiety, and cognitive disturbances, and how these symptoms arise is not fully understood or predictable. If doctors could better predict who would develop PTSD, they would be able to potentially improve treatments and outcomes.
Researchers set out to use magnetic resonance imaging (MRI) to find potential brain biomarkers of PTSD in people with traumatic brain injury (TBI).
“The relationship between TBI and PTSD has garnered increased attention in recent years as studies have shown considerable overlap in risk factors and symptoms,” said lead author Murray Stein, MD, MPH, FRCPC, a Distinguished Professor of Psychiatry and Family Medicine & Public Health at the University of California San Diego, San Diego, La Jolla, CA.
“In this study, we were able to use data from TRACK-TBI, a large longitudinal study of patients who present in the Emergency Department with TBIs serious enough to warrant CT (computed tomography) scans.”
Researchers followed over 400 TBI patients, assessing them at three and six months after their brain injury. At three months, 77 participants – or 18 percent – had likely PTSD. At six months, 70 participants, or 16 percent, did. All subjects underwent brain injury after injury.
“MRI studies conducted within two weeks of injury were used to measure volumes of key structures in the brain thought to be involved in PTSD,” said Stein. “We found that the volume of several of these structures were predictive of PTSD three-months post-injury.”
Specifically, smaller volume in brain regions called the cingulate cortex, the superior frontal cortex, and the insula predicted PTSD at three months. The regions are associated with arousal, attention, and emotional regulation. The structural imaging did not predict PTSD at six months.
Researchers noted that these results align with previous studies showing smaller volume in several of these brain regions in people with PTSD and studies suggesting that the reduced cortical volume may be a risk factor for developing PTSD.
Together, the findings suggest that a brain reserve, or higher cortical volumes, may provide some resilience against PTSD.
The biomarker of brain volume differences is not yet robust enough to provide clinical guidance, but the team pointed out that the findings could inform further research.
“The findings do pave the way for future studies to look even more closely at how these brain regions may contribute to (or protect against) mental health problems such as PTSD,” Stein said.
The results of the study demonstrate the ability of medical imaging to help improve PTSD diagnosis and treatment.
“This very important study uses magnetic resonance imaging to take the field a step closer to understanding why some people develop PTSD after trauma and others do not,” said Cameron Carter, MD, Editor of Biological Psychiatry: Cognitive Neuroscience and Neuroimaging.
“It also lays the groundwork for future research aimed at using brain imaging to help predict that a person is at increased risk and may benefit from targeted interventions to reduce the clinical impact of a traumatic event.”
This study adds to recent efforts to enhance PTSD diagnosis. In October 2020, researchers from Boston University School of Public Health (BUSPH) used machine learning to cut six of the 20 questions used to diagnose PTSD while still maintaining accuracy in a veteran population.
“We found that several of the PTSD items could be removed because they did not make substantial contributions to accurate prediction of PTSD relative to the other PTSD items. It's likely that some of these items are removable because they are redundant with other items. Other items may be removable because they aren't specific enough to PTSD,” said study lead author Tammy Jiang, a doctoral candidate in epidemiology at BUSPH.
